Abstract
Acute graft-versus-host disease remains a significant cause of morbidity and mortality after allogeneic hematopoietic cell transplantation (HCT). Grade III-IV aGVHD is associated with a high short-term morbidity and a dismal prognosis. Associated late effects in patients who recover from grade III-IV aGVHD are unknown.
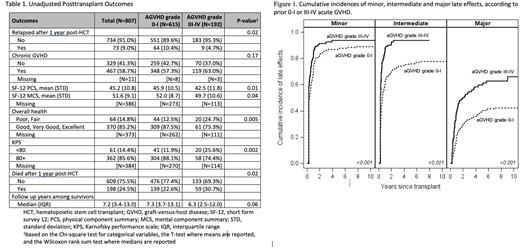
The objectives of this study were to analyze late medical comorbidities, quality of life, non-relapse mortality and survival in patients who recovered from grade III-IV aGVHD. Chart review identified late effects. Patients were asked to complete annual surveys to collect patient reported outcomes (PRO), including self-reported Karnofsky performance scale (KPS) and general health. The average response per patient was used for the analysis. Late medical comorbidities were grouped into minor, intermediate and major based on usual degree of morbidity associated with each condition. Only medical conditions starting after HCT were included. Outcomes were compared between patients with grade III-IV aGVHD and those with grade 0-I aGVHD (controls) who were transplanted between 2001-2019 and survived at least one year after HCT without recurrence of malignancy. Patients with grade II aGVHD were excluded given the focus on severe aGVHD and the intermediate prognosis associated with clinically heterogeneous grade II aGVHD.
There were 192 patients with grade III-IV aGVHD and 615 patients with grade 0-I aGVHD. The median follow-up time was 7.2 years (interquartile range 3.4 - 13.0). Patients with a history of grade III-IV aGVHD had significantly higher rates of late medical comorbidities (minor HR 1.11 95% CI 1.04-1.19, intermediate HR 1.27 95% CI 1.19 - 1.36, major HR 1.27 95% CI 1.16-1.39, p <0.001, Figure 1) and worse physical (p=0.01) and mental (p=0.04) functioning compared to patients who only had grade 0-I aGVHD. Patients with grade III-IV aGVHD were more likely to report poor or fair health (24.7% vs 12.5%, p=0.005) and a KPS of 70 or lower (25.6% vs. 11.9%, p=0.002) than those with grade 0-I aGVHD.
Patients who survived >1 year post-transplant and had prior grade III-IV aGVHD also had worse 5-year overall survival (OS) (77.5% vs. 83.6%, p=0.006) and higher non-relapse mortality (NRM) (19.2% vs. 10.6%, p <0.001) than those with a history of grade 0-I aGVHD. No difference was found in cumulative incidence of chronic GVHD (Table 1) which may be due to exclusion of grade II and the relatively small number of grade III-IV aGVHD patients.
In conclusion, patients who recover from severe aGVHD remain vulnerable to developing late comorbidities. They continue to have higher rates of NRM and lower OS compared to patients who had grade 0-I aGVHD. These patients would likely benefit from continued monitoring and supportive care to try to prevent late effects and improve survival.
Disclosures
Krakow:HighPass Bio: Research Funding. Lee:Amgen: Research Funding; AstraZeneca: Research Funding; Incyte: Research Funding; Kadmon: Consultancy, Honoraria, Research Funding; Pfizer: Research Funding; Syndax: Research Funding; Mallinckrodt: Consultancy, Honoraria; Equillium: Consultancy, Honoraria; Novartis: Other: Steering Committee; National Marrow Donor Program: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal